Legislative Matters
The Ethical Guidelines (NHMRC) inform ethical practice for health professionals in relation to eligibility criteria for entry onto organ transplant waiting lists, donor suitability criteria for organ allocation for transplantation, and the organ allocation protocols for determining transplant recipients. –
See more at: http://www.donatelife.gov.au/clinical-and-ethical-guidelines-organ-transplantation-deceased-donors
Kidney Donor
Living donors have donated an organ or bone marrow to another person to help save their life and improve their general health and wellbeing.
Prospective living donors are worked up in details to ensure that no harm is done to the donors from their decision.
Renal donors need long-term follow-up to ensure the optinmal functioning of the single remaining kidney.
This section provides information for both scenarios
Recipient
Transplantation remains the best option for majority of the patients with Advanced Chronic Kidney Disease; who do not have significant comorbidities that impact on their survival.
However, limited donor organs remains a challenge; needing promotion of kidney donation from living friends and relative; AND allocation of the organs from deceased donor according to the state-wide criteria.
Becoming a LIVING donor
Organ and tissue donation saves lives. That is the simple truth. Risks of being a kidney donor are small but should be considered seriously.
The feeling of satisfaction for the donor is a very positive psychological experience knowing that he or she has helped save the life of someone in need. There is no way to measure this benefit but it is very real to the people that experience it.
To find out information on becoming a living kidney donor visit:
- Are you ready to be a KIDNEY Donor? http://kidney.org.au/cms_uploads/docs/deciding-to-be-a-living-kidney-donor-fact-sheet.pdf
- What is involved in the LIVING KIDNEY DONATION? http://kidney.org.au/cms_uploads/docs/living-kidney-donation-fact-sheet.pdf
- Can I give be a KIDNEY DONOR to someone on the kidney transplant waiting list? In this situation you do not know the person who receives your kidney. http://kidney.org.au/cms_uploads/docs/non-directed-living-kidney-donation-fact-sheet.pdf
For more information about your suitability, intent or other issues, talk to your doctor.
SHORT TERM RISKS of kidney donation
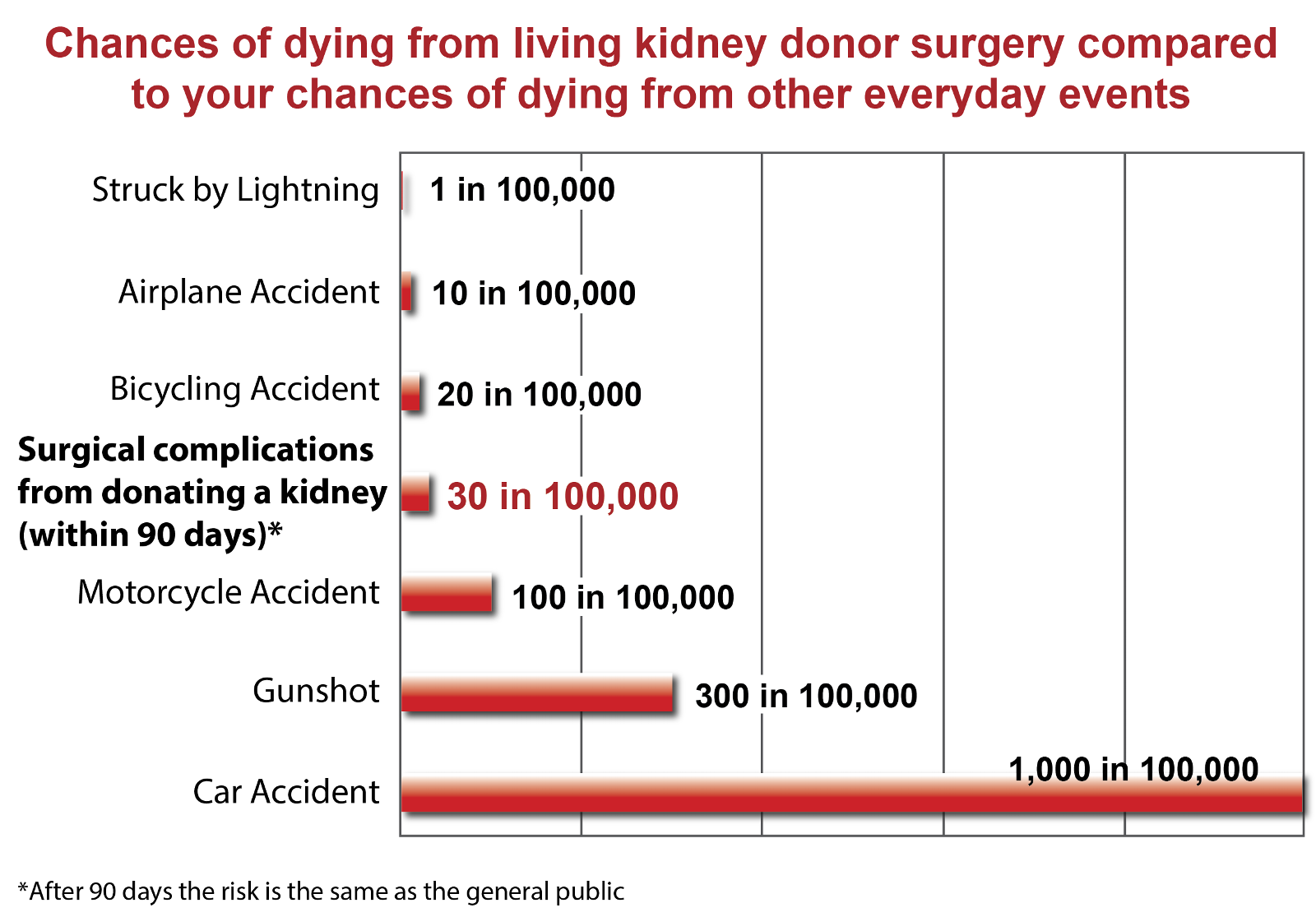
One of the main issues a donor will face is the risk of major surgery. All surgery carries risks, no matter how small.
The most common risks associated with a nephrectomy are usually relatively minor and can be treated appropriately.
Major surgical complications include:
- Wound, urinary tract and chest infections, which occur in approximately one in three (33%) donors.
- Bleeding that requires blood transfusion or blood clots, occur in approximately one in 50 (2%) donors
- Rarely, one in 3,300 donors die as a result of the operation.
- The most common causes of death are pulmonary embolisms (blood clot in the lung) or heart attack.
- However, the chance of this happening has been compared to the risk of having a fatal road accident.
- The most common causes of death are pulmonary embolisms (blood clot in the lung) or heart attack.
- Pain, scarring (not with newer laparoscopic methods), bloating and other symptoms can be managed medically.
For more information:
Long Term Risks Of Kidney Donation
It is generally considered very safe to live with one kidney and your doctors and their teams will outline the main risks to you.
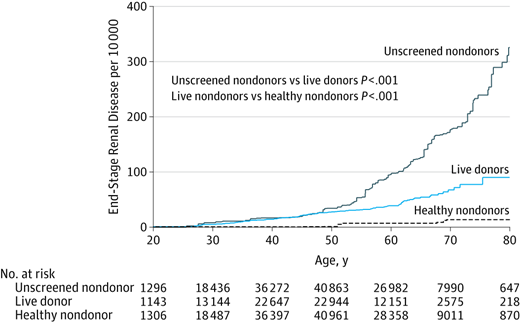
It is important to note that studies into the long-term effects of donating a kidney are on-going. Considering one kidney, donors have low reserve and thus remain at risk for marginally higher rates of kidney disease (especially immunologic diseases) and probably death with a small magnitude over many years of follow-up; as compared to screened healthy donors who were no transplanted. The risks of death and kidney disease is much lower in the donors than in the un-screened general population.
It is important to be aware that every donation carries risks and it is not possible to cover every eventuality when considering risk. However, some of the most notable post-donation research indicates the following:
- Some studies have indicated that there is a slightly higher chance of a small increase in your blood pressure or the amount of protein in your urine as a result of having one kidney. However, these are checked at annual follow-up and, if found, can be treated.
- The overall risk of developing significant disease in your remaining kidney after donation is low, occurring in fewer than one in 200 (0.5%) donors, and it is much less in kidney donors than it is in the general (unscreened) population (because kidney donors are, of course, pre-screened to ensure they are healthy).
- Compared to the general public, most kidney donors have equivalent (or better) survival, excellent quality of life, and no increase in end-stage renal disease (ESRD – kidney disease).
- However, some studies have indicated a slightly increased incidence of ESRD post-donation among certain groups, in particular, black donors, younger donors, donors genetically related to their recipients, donors related to recipients with immunological causes of their renal failure, and overweight donors. However, the risk is still lower than that of the general (unscreened) population.
- Whilst most women have uncomplicated pregnancies after donation, there is a slightly increased risk of gestational hypertension or pre-eclampsia.
- It is also important to be aware that, although generally risks across the board are very low, every individual is different and it is not impossible for a number of other uncommon complications to occur. For example, although rare, on-going fatigue and persistent pain have been reported by small numbers of the thousands of living donors.
You can check the latest professional guidelines on the British Transplantation Society website.
Resources for donors within Australia and WA

Supporting Living Organ Donors Program
- The Supporting Living Organ Donors Program (the Program) seeks to raise the profile of living organ donors and also encourage employers to support donors.
- The aim of the Program is to ensure that cost is not a barrier for living organ donors to donate a kidney or part of their liver by providing a financial contribution to employers to either replenish an employee’s leave or contribute towards reimbursing an employer who has made a payment to their employee in place of income lost due to organ donation.
- On 8 May 2017, the Australian Government announced that the Program would continue for four years from 1 July 2017 with some important changes.
- From 1 July 2017, the program has been expanded to allow donors who are having surgery on or after this date to claim reimbursement for some out of pocket expenses, enabling donors who are not employed to participate.
Eligibility and payment rates
- To be eligible for the Supporting Living Organ Donors Program, the donor must be:
- an Australian citizen or permanent resident with a valid Medicare card;
- 18 years of age or older;
- intending to donate a kidney or partial liver;
- donating in Australia*; and
- (if seeking reimbursement for leave taken) employed by:
- a registered Australian business with an active ABN; and
- an employer willing to participate in the Program (or be self-employed with an active ABN).
- The Program provides a payment of up to nine weeks, based on a 38 hour week (a maximum of 342 hours), at up to the National Minimum Wage.
- As at 1 July 2017, the National Minimum Wage is $694.90 per week, or $18.29 per hour, as determined by the Fair Work Ombudsman.
- If surgery was prior to 1 July 2017, you are unable to claim any out-of-pocket expenses.
The Department of Health has made every effort to ensure that the documents on this web page meet accessibility requirements. If you are experiencing difficulty accessing the information contained within any of these document, please contact livingorgandonation@health.gov.au or call (02) 6289 5055 to arrange for an alternative format to be provided to you.
Program Documents
- For donors and employers who are interested in the Program please see the Guidelines for further information.
- Frequently Asked Questions about the Program are available.
Registration
- If you are undergoing surgery between 1 July 2017 and 30 June 2021 to donate a kidney or part of your liver, please complete the Individual Registration Form and return it, and relevant supporting documentation, to the Department of Health via post:Supporting Living Organ Donors Program
Department of Health
GPO Box 9848
CANBERRA ACT 2601 - Individual Registration Form – PDF 153 KB
Individual Registration Form – Word 133 KB - Alternatively, you can scan and email a copy to: livingorgandonation@health.gov.au
- If you do not have access to a printer, call us on (02) 6289 5055 and we can mail a form to you.
- The completed form should be submitted prior to commencing your leave. Once your form has been received, we will assess your eligibility and notify you and your employer separately in writing.
Claiming
- If you are deemed eligible, we will send:
- to you – an Individual Claim Form, Out-of-pocket expenses tracker, and Appointment sign-off sheet;
- to your employer – an Employer Payment Form to submit once you have returned to work; or
- to self-employed donors – a Self-Employed Claim Form, Out-of-pocket expenses tracker, and Appointment sign-off sheet.
The Individual Claim Form, Employer Payment Form, Self-Employed Claim Form, Out-of-pocket expenses tracker, and Appointment sign-off sheet are available to download
-
- Individual Claim Form – PDF 128 KB
- Individual Claim Form – Word 105 KB
- Employer Payment Form – PDF 120 KB
- Employer Payment Form – Word 101 KB
- Self-Employed Claim Form – PDF 131 KB
- Self-Employed Claim Form – Word 129 KB
- Out-of-pocket expenses tracker – PDF 100 KB
- Out-of-pocket expenses tracker – Word 144 KB
- Appointment sign-off sheet – PDF 86 KB
- Appointment sign-off sheet – Word 42 KB
- When a donor has completed their leave and been paid for their time off, the Individual Claim Form, Employer Payment Form (or Self-Employed Claim Form) can be completed and returned with relevant supporting documentation to the Department of Health (to the same address as above).
- The donor and their employer will be notified of the outcome after all documentation has been received and assessed.
Change of Circumstances
It is important you tell us if your circumstances change. By keeping us up-to-date, we can accurately assess your circumstances. For example, if:
- your personal details change
- you change your address or phone number
- your employment changes
- your medical practitioner changes, or
- you have decided to not go through the donation process.
Feedback
- If you have any questions or feedback about the Supporting Leave for Living Organ Donors Program, please email livingorgandonation@health.gov.au
- Further information about living kidney donation can be found at Kidney Health Australia’s website
Pilot Program
- Living donors who underwent surgery between 1 July 2013 and 30 June 2015 are no longer eligible to apply under the Program.
- The Program pilot started on 1 July 2013 and ended on 30 June 2015. For that two-year period, the Department of Human Services administered the Program.
- ACIL Allen Consulting conducted an evaluation of the pilot. The final report was provided to the Department of Health in December 2014.
- Payments under the pilot were for an amount up to the National Minimum Wage for up to six weeks of leave.
For general enquiries please email: livingorgandonation@health.gov.au or call (02) 6289 5055.
The Department of Health has made every effort to ensure that the documents on this web page meet accessibility requirements. If you are experiencing difficulty accessing the information contained within any of these document, please contact livingorgandonation@health.gov.au or call (02) 6289 5055 to arrange for an alternative format to be provided to you.
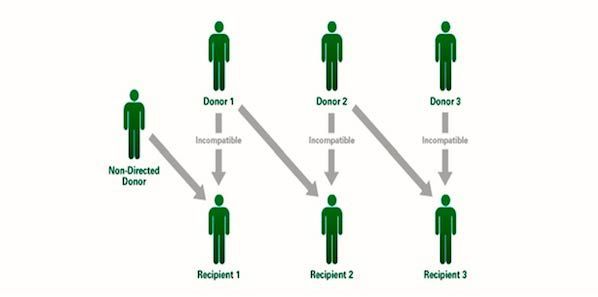
Non- Directed (Altruistic) Donation
- In Non-directed living kidney donation, you donate a kidney to someone on the kidney transplant waiting list.In this situation you do not know the person who receives your kidney. Being a non-directed living kidney donor is a very serious decision.National guidelines for deciding who will receive a donated organ or tissue in Australia, can be seen on the Transplantation Society of Australia and New Zealand website www.tsanz. com.au/Non-Directed donation has improved the living kidney donation by many folds due to its use in Australian Paired Kidney Exchange Programme, across multiple states triggered from one donor.
For more information:
http://kidney.org.au/cms_uploads/docs/non-directed-living-kidney-donation-fact-sheet.pdf